Parents of Highly Sensitive Children
Parents of Highly Sensitive Children...
Your child is constantly exploding (or imploding). And you are ready to stop following basic gentle parenting that doesn’t match your kid, design an individualized, systematic approach to eliminate your kid’s explosive meltdowns and finally raise a resilient, emotionally intelligent child.

Hi there!
Megghan
Thompson
LCPC, RPT-S
I train parents to eliminate daily meltdowns for their sensitive children so the whole household can go from reactive to resilient... and we do that in as little as 8 weeks.
You know you can solve this problem, but you haven't figured it out yet. And now, you secretly worry about feeling like a hostage to your child's emotions in your own home. This is not your fault.
It's simple, we help awesome parents with awesome kids learn effective skills... without getting another Master's Degree. In working with us, parents efficiently develop critical thinking skills to apply child development neuroscience to finally foster psychological safety in their homes.
It's your time to thrive!

Featured on...




Ready to feel less like a puppet to your child’s outbursts?
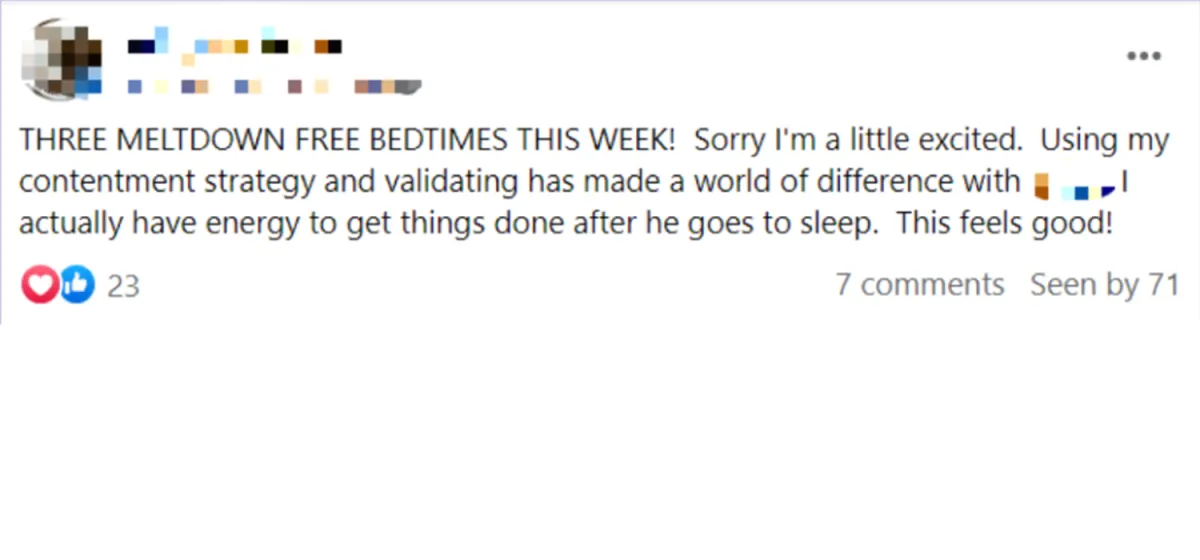
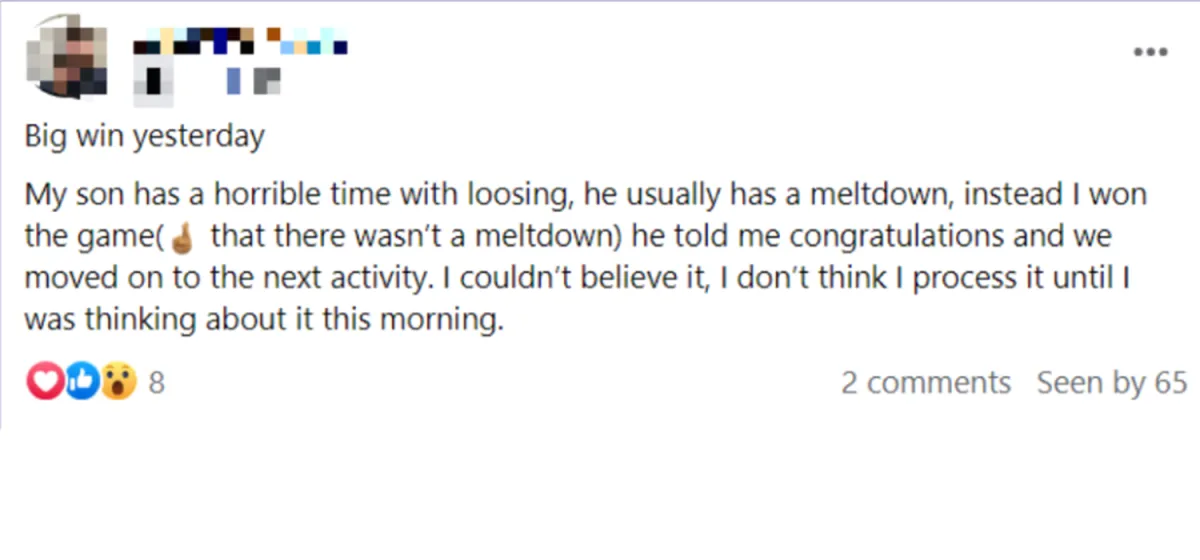
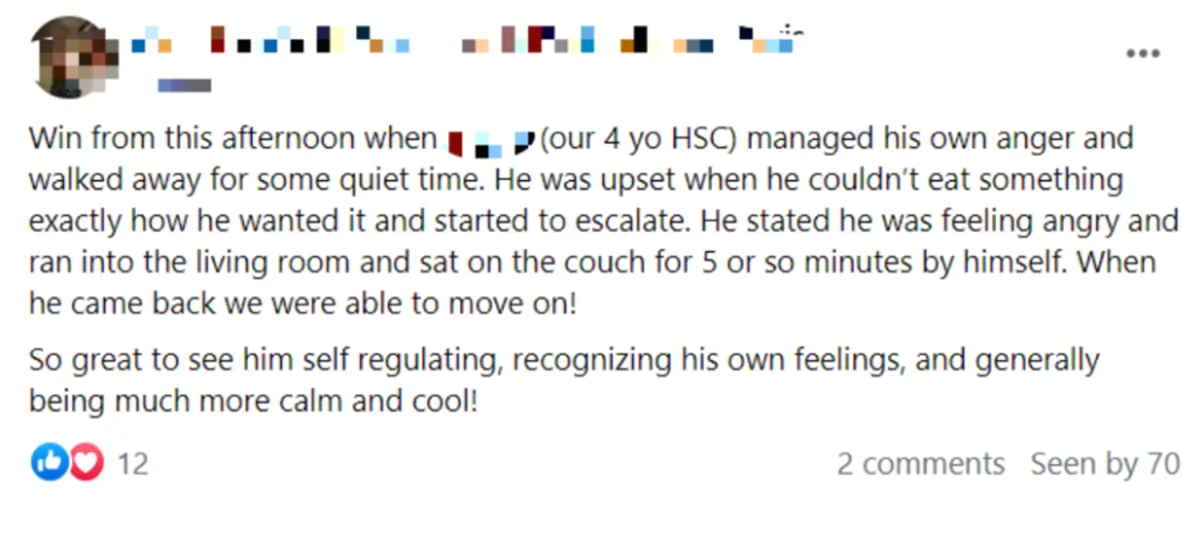
Join me in the Parent Your Highly Sensitive Child Like a Ninja Facebook group for parents. You’ll gain skills that will help you feel capable and confident disciplining your child while helping your child feel understood in a world that says they are “too much.”
I give weekly trainings on raising children who don’t fit the mold of the typical parenting books.




Fast, Lasting Results

Sign up for exclusive content, emails & things Megghan doesn’t share anywhere else.
Copyright © 2018-2025 Megghan Thompson Coaching